Marbled skin
SYMPTOMS
What are the manifestations of cutis marmorata?
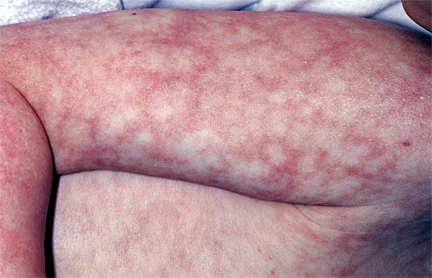
Cutis marmorata refers to a marbled appearance of the skin characterized by purplish-red or light blue reticulated patches.
Its hallmark is symmetrical reticulated patches on the limbs and trunk (as shown in Figures 1 and 2).

(Figure 1 source: UpToDate Clinical Advisor)
(Figure 2 source: UpToDate Clinical Advisor)
What causes cutis marmorata?
Cutis marmorata can result from various causes, including physiological, congenital, secondary, or idiopathic (unknown origin).
-
In newborns, physiological or congenital cutis marmorata is more common. In neonates and children, it may also occur secondary to critical illnesses such as severe infections, respiratory/circulatory failure, or early-stage shock.
-
In adults, it is often secondary to other factors but may also be physiological or idiopathic.
What are the types of cutis marmorata, and what are their characteristics?
The primary mechanism of cutis marmorata involves spasms of vertically oriented arterioles in the dermis, leading to dilation of capillaries and venules, slowed blood flow, hypoxia, and the appearance of bluish-purple reticulated patches.
- Physiological cutis marmorata
This occurs in 50% of normal children and adults and is typically visible throughout infancy.
Exposure to cold triggers temporary red-blue reticulated patches, mostly on the lower limbs and trunk, which disappear upon warming. The exact cause remains unclear.
- Congenital phlebectatic cutis marmorata
Also known as congenital livedo reticularis, this condition appears at birth or shortly after, presenting as persistent purplish-red or bluish reticulated patches due to venous and capillary dilation, resembling marble patterns. Symptoms may worsen with cold exposure or crying.
Lesions are often unilateral, segmental, or localized, primarily affecting the limbs, followed by the trunk, face, and scalp. Affected skin may atrophy, ulcerate, or leave atrophic scars (Figure 3).
Most lesions improve with age, often fading or resolving within two years, though rare cases may persist long-term.

- Secondary cutis marmorata
This type arises secondary to pathological conditions. In children, it often appears as "mottling" or "marbling," signaling severe illnesses like infections, respiratory/circulatory failure, dehydration, or early shock.
If mottling occurs during illness, prompt medical attention is required.
In adults, it is usually secondary to underlying diseases or medications, presenting as asymmetric patches, such as in vascular obstruction or vessel wall disorders.
- Idiopathic cutis marmorata
This type has no known cause and mainly affects young and middle-aged women. It is typically mild and harmless, sometimes coexisting with physiological livedo reticularis. Symptoms begin in the 30s–40s, initially triggered by cold and transient, later becoming persistent with tingling or numbness. The condition may remain stable or progress.
Severe cases may develop ulcers, often in winter (though they can appear suddenly in summer), located around the ankles and dorsum of the feet. These ulcers are irregular, 1–5 mm in diameter, varying in depth, and may be accompanied by ecchymoses, hemorrhagic papules, blisters, or subcutaneous nodules. Healing is slow, leaving white atrophic scars.
TREATMENT
Does Marble-like Skin Require Treatment?
-
Physiological and uncomplicated idiopathic marbled skin should avoid cold exposure and keep warm, with no active treatment needed. It does not affect daily life or diet.
-
Congenital livedo reticularis also has no specific treatment. Most skin lesions gradually improve with age, typically fading or resolving within 2 years, though rare cases may persist long-term. Associated malformations can be managed accordingly.
-
Severe cases, including those with ulcers, may benefit from long-term anticoagulant, antifibrinolytic, or thrombolytic therapy.
-
Secondary cases require identifying the underlying cause, treating the primary condition, and discontinuing causative medications.
-
If marbled skin suddenly appears in a child during illness (not due to cold) or is accompanied by abnormal mental status or reactions, prompt medical attention is necessary.
DIAGNOSIS
Which department should I visit for marbled skin?
Dermatology. Children should first visit the pediatrics department.
How to distinguish between physiological and congenital marbled skin?
Physiological marbling disappears on its own when the limbs are warmed, whereas congenital skin abnormalities typically do not fade with rewarming and exhibit coarser vascular patterns, distinguishing them from physiological cases.
Histopathological examination may be necessary for differentiation. Physiological marbled skin shows normal histology, while congenital cutis marmorata telangiectatica presents significant capillary dilation, sometimes accompanied by venous dilation, vascular fibrosis, lymphatic dilation, or venous thrombosis.
POTENTIAL DISEASES
In which abnormal diseases can marbled skin be observed?
Marbled skin in children is mostly physiological or congenital. Its appearance during illness indicates a severe condition.
Reports suggest that 27%–80% of cases are associated with other abnormalities, including capillary malformations, body or limb asymmetry, glaucoma (especially with facial involvement), congenital localized skin aplasia, cleft palate or other deformities, and migraines.
Secondary causes include intravascular obstruction and vascular wall diseases:
-
Intravascular obstruction: Blood stasis (e.g., paralysis, heart failure, amantadine treatment); occlusive diseases (e.g., embolism, oxalosis, decompression sickness in divers, drug-induced—bismuth, pentazocine, NSAIDs, minocycline), thrombocytopenia, cryoglobulinemia, polycythemia, thrombocythemia, cold agglutinin disease, macroglobulinemia.
-
Vascular wall diseases: Arteriosclerosis; arteritis (e.g., polyarteritis nodosa, lupus erythematosus, rheumatoid arthritis, dermatomyositis, lymphoma, mycosis fungoides, breast cancer, pheochromocytoma, pancreatitis); infections (e.g., pneumococcal sepsis, tuberculosis, syphilis, hepatitis C, brucellosis, Coxiella burnetii infection, parvovirus B19, meningococcemia); hyperparathyroidism and hypercalcemia (e.g., calciphylaxis); others include hypertension, erythema ab igne, carbon dioxide arteriography, photosensitivity, quinidine use, etc.